ABSTRACT: Working with patients who have suffered from an accident or injury and their families at KAT Attica General Hospital in Greece, we often faced a loss in the patient's body causing chain reactions in the wider body of the family. What particularly struck us was the fact that the physical disability (paraplegia, quadriplegia) that followed the injury, although it was initially enrollable at a level of randomness under the influence of external unpredictable factors, in the process was associated with the family dynamic. In the case of the 20 families studied, the patient's body brought to the surface conflicts, dysfunctional developmental transitions and crises that the family was trying to forget. The main purpose of this qualitative research was to associate the high levels of expressed emotion, which were observed in family and measured by the Five-minute Speech Sample, with the physiological rehabilitation of the patient.
Key words꞉ paraplegia, quadriplegia, accident, expressed emotion
Introduction
For several decades, research has focused on families' understanding and response to a variety of illnesses and health conditions, to the specific characteristics of illness and their relative impact on the family, and on the ways families approach short- and long-term disease management. In this direction, the "Expressed Emotion" (Expressed Emotion) index emerged as a method measuring interpersonal attitudes. Expressed Emotion (EE) refers to a “construct” that represents some central aspects of interpersonal relationships and involves measures of hostility (generalized criticism or rejection), criticism (overt dislike or disapproval of behavior), and emotional overinvolvement (emotionally excessive or self-sacrificing behavior) on the part of a significant person – usually a family member – towards the patient. Then, because levels of hostility were found to be related to levels of criticism, studies focused on criticism and on emotional overinvolvement as components of EE (Barrowclough & Hooley 2003; Van Wearden et al. 2000).
The research actually began in 1959 and involved 229 patients discharged after two or more years of hospitalization (Brown, 1959). In this study, a significant relationship emerged between the recurrence of schizophrenia symptoms and the type of family environment the patient returned after the discharge. The second study by Brown and colleagues in 1962 investigated the "emotional involvement" of the schizophrenic patient's family and claimed that one year after discharge 3/4 of the patients who returned to families with "high emotional involvement" relapsed whereas of the rest relapsed less than 1/3. The need to define the concept of "emotional involvement" and its importance led to the design of the next study focused on the construction of measurement tools from which emerged the first research tool aimed at capturing the whole range of emotions encountered in ordinary families, the standardized semi-structured Camberwell Family Interview (CFI) (Wearden et al., 2000). Using the CFI, Brown and colleagues (1962) argued that the best predictor of relapse in schizophrenia after the patient's discharge is the expressed emotion of the relative living with the patient.
In recent years research has shown that family-patient interaction is associated with the patient’s outcome in a range of psychiatric (Brown et al., 1959) and medical conditions (Wearden et al., 2000). High EE is a reliable psychosocial predictor of relapse in schizophrenia, mood disorders (Butzlaff & Hooley, 1998), and alcohol dependence (Fichter, et al., 1997). It also predicts worse outcomes for patients with anxiety (Fogler et al., 2007), eating disorders (Zabala et al., 2009), increased depression and in patients with medical conditions such as epilepsy, myocardial infarction (Bressi et al., 2009), diabetes (Wearden et al., 2000), and stroke (Weddell et al., 2010). Most studies have found a correlation between family expressed emotions and patient’s relapse.
Relatives of patients with high levels of EE adopt a rigid perspective. They believe that patients can control the symptomatology associated with their illness and thus develop a critical attitude arguing that only through this will the patient change their behavior (Wearden et al., 2000). They criticize behaviors that are not related to the patient's health condition but more to the individual and this often leads to relapse and regression. Other family members believe that the symptoms are out of the patient's control and develop high levels of emotional over-involvement in an attempt to reduce their impact (Barrowclough & Hooley, 2003). These families constantly blame themselves, any negative event is seen as their fault and they become overly involved because there is a sense of pity towards the sick family member. These relatives become so unbearable that the patient can no longer live with this kind of anxiety and regresses to the illness to manage and cope with the new reality.
Research Data
Anxiety and depression often occur after severe injuries and have a negative impact on the patient's recovery. Recent research has found prevalence rates of 44.1% for anxiety disorders and 29.4% for major depressive disorders in the first year after injury (Gould et al., 2011). The researchers note the need to further examine the contribution of psychosocial factors that may respond to early intervention such as the family's ability to effectively support the injured person's recovery.
There are no research data examining the relationship between the physical rehabilitation of the paraplegic/quadriplegic patient with brain damage and the EE in his family. Typical is the research of Weddell (2010) in which, in a sample of 78 patients with severe brain damage found that one aspect of EE -criticism- was significantly associated with the depression of these patients, and more specifically depression levels were found to increase and be related with the presence of a critical member in the family. If the patient does not have a family of his own, he often returns to his paternal family after his injury and the atmosphere there will affect his adaptation and rehabilitation. Once criticism and emotional over-involvement appear, the family gets trapped in a vicious cycle of interactions that creates more problems than the disability itself.
The effect of EE has been studied mainly in depressed patients and the majority of researchers have concluded that these patients tend to attribute negative life events to themselves. So when relatives become critical and attribute negative events to internal factors of the patient, they reinforce their beliefs and consequently their sensitivity and responsiveness to the criticism (Wearden et al. 2000).
Method
Demographic Characteristics of Patients and Relatives
Our study involved 20 patients with incomplete or complete damage (paraplegia, quadriplegia) who were undergoing rehabilitation at the KAT Hospital in Athens and had suffered a traumatic brain injury (TBI) which did not affect their cognitive function.
The patients’ ages ranged from 14 to 65, the majority were male (80%), the time after injury ranged from 15 to 120 days, and 50% of the patients had quadriplegia and traumatic brain injury that did not affect their cognitive function.
The ages of the family members ranged from 40 to 73. Mostly parents (60%) but also spouses (40%) of the patients who lived with them and were responsible for any additional daily support they needed. The frequency of their contact with the patient was daily .
Measuring Tools
Five Minutes Speech Sample (5MSS)
The Five-Minute Speech Sample (5MSS) (Gottschalk & Gleser, 1969) is a short EE measurement focusing on four categories: 1. quality of initial statement, 2. quality of relationship, 3. critical mood/attitude, and 4. over involvement.
An initial statement is defined as the first complete thought or idea expressed by the respondent about the patient. A relationship statement is defined as the comment made about the relative-patient relationship, which expresses a complete thought. The critical mood occupies the entire speech and emotional over involvement occurs through overprotective behavior, emotional exposure and excessive detail in the in the relative's information about the patient.
The HADS Hospital Anxiety and Depression Scale (Zigmond & Snaith, 1983)
The questionnaire consists of seven items reflecting anxiety (HADS-A) and seven reflecting depression (HADS-D). Each item receives a 4-point response (0–3) while total scores for each subscale range from 0 to 21 and are classified as normal (0–7), mild (8–10), moderate (11–14), or severe ( 15–21).
Results
HADS scale
56.5% of patients reported mild anxiety (score 8–10), 18.9% moderate (score 11–14) and 9.2% severe anxiety (score 15–21). On the depression scale, 67.9% of patients had mild symptoms and 4.5% had moderate symptoms.
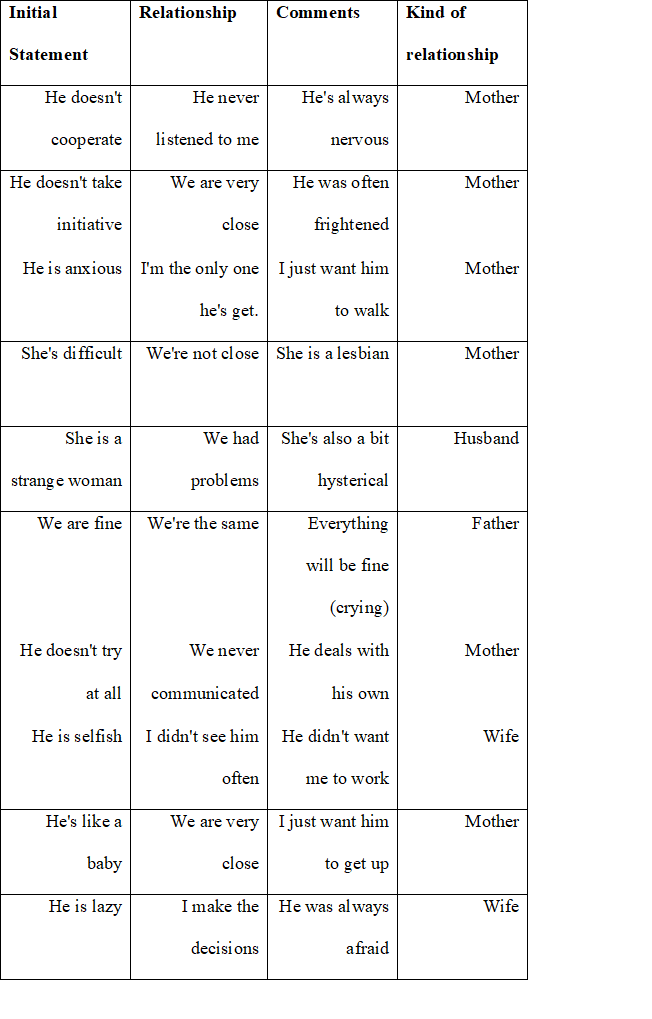
5 FMSS
A. critical attitude/criticism
A relative can be characterized as having a high EE in critical attitude if he or she makes a negative initial statement, one or more critical comments assessed either on the content or tone of voice, and report overall negatively to the relationship. Of the 20 families, 17 were classified as high EE (85%) and 3 as low (15%). Some examples of the initial statement, relationship and comments are shown in table 1.
B. Emotional Overinvolvement (EOI)
A relative is defined as having a high EE on the EOI if he/she exhibits an emotional display during the interview (eg, crying), an overprotective or self-sacrificing behavior, and displays two or more of the following characteristics: exaggerated details from the past, one or more statements of his/her attitude and five or more positive comments.
Of the 17 relatives rated as high EE in critical attitude, 15 presented an emotional display during the interview (eg, crying), 12 provided excessive details about the patient about minor aspects of his/her behavior (such as a detailed description of patients' involvement with mobile phone) displaying a tendency to dramatize and 11 showed an excessive emotional reaction (“I'm so worried that I'll get sick too”). Finally recorded 13 reports of overprotection (“I constantly wonder if I've done something wrong, I am afraid to let him eat or dress himself”).
Discussion
The family therapy movement during the 1950s initially focused on the family of the schizophrenic, and many researchers linked the cause of the disorder with certain "pathogenic" types of family communication. Today scientific research has demonstrated the important role of the family in both vulnerability to the disease and in its adaptation, course and recovery. The need to identify and evaluate the factors that contribute to the formation of the emotional domestic atmosphere has led to the development of various tools from which expressed emotion is mainly used. The way family members perceive the illness is internalized by the patient and if it is negative it can add undue stress and depression that has short and long term effects on the use of health and welfare services, disability status, and quality of life (Wearden et al. 2000). In recent years, a variety of therapeutic approaches have used the concept of EE, designing interventions that mainly concern psychoeducation, multiple family therapy, behavioral family therapy, and systemic therapy. These interventions aim at educating the family about the disease, improving communication, managing the crisis and helping patients and relatives express their negative feelings in more constructive ways. (Tomaras & Mavreas, 1990).
Although EE is now an important part of Clinical Research, few are known about the factors that determine it. Does it represent an established model of family interactions or is it a response to a stressful stimulus such as the disability and increased care needs of these patients? Is it related to some specific characteristics of the patients themselves or does it reflect an underlying pathology of family functioning? Research data often show contradictory results, some studies link high EE to patient variables such as longer disease duration (Stirling et al. 1991), poorer social functioning and greater symptom severity (Glynn et al., 1990), while others with some characteristic disturbances in communication and interaction, with less marital satisfaction (Marks et al., 1996), with more negative life events, with greater family conflict or even with poorer overall family functioning (Wamboldt et al., 2000).
There are not yet enough research findings that allow safe conclusions to be drawn about the predictive power of EE in various medical and health conditions. In the present pilot study, the majority of patients presented mild symptoms of anxiety (56.4%) and depression (67.9%) and the majority of their relatives (85%) were classified as high EE. As there is not enough research data on this specific topic, this study mainly aimed to show that the EE methodology can be successfully adapted to examine the role of families in the course and outcome of patients with quadriplegia and paraplegia and that there are associations, between EE and disease outcomes that are worth pursuing. Uncovering different patterns of EE in disability may help to understand the origin and meaning of the family’s expressed emotions.
The differences between low and high expressed emotion families are striking. It seems that relatives with low EE support the patient actively, provide positive non-verbal climate and try to find solutions to the problems. They perceive that the patient is facing a difficult situation and needs support rather than criticism to overcome the obstacles they face. In contrast, relatives who score high on EE tend to be trapped in chains of repetitive negative interactions and have problems communicating with the patient as they talk more and listen less effectively.
In the disability, the relative will be faced with symptoms that people without the impairment do not have and for which there is a medical explanation. While the patient's behavior may be considered to affect the illness (e.g. a relative may believe that the patient has more symptoms because he is not compliant with treatment and rehabilitation) and the disability may be considered to influence the patient's behavior (e.g a relative may think that certain aspects of it make the patient irritable), it is not the patient's behavior that is actually the problem. There is therefore the possibility of an additional layer of causation to explain any family dysfunction that occurs and that may be EE.
In clinical research, the same dimensions of high EE lead to dysfunctional causal associations related to the disease and the patient's control over it, affecting rehabilitation and treatment. The anxiety from the family's observations and behaviors is overwhelming and patients feel they are the cause of all the problems. The only way for the family to get out of this mess and improve their quality of life is to go through therapy and support which help them cope with the situation with less stress and discomfort. Injury of the patient's body causes chain reactions in the wider body of the family. In order to restore and manage this injured body, the family must be supported in order to face and manage the new existential reality that arises. Reducing expressed emotion and educating the family about physical illness and disability will increase understanding and acceptance, improve family interactions, prevent conflict, and help heal trauma.
Suggestions for future research
The contribution of the EE to the course of the disease in medical conditions and disability has not yet been determined. Most of the studies that have been conducted have been cross-sectional in nature and cannot lead to any safe conclusions about the long-term association between the EE and the outcomes of the disease. Undoubtedly the EE is an additional stressful factor for the patient but with the so far available data, it is difficult to present a comprehensive model of intervention. Therefore research and systemic therapy are called to examine more the EE and its role in mental and physical medical conditions as well as in the patients’ rehabilitation after injuries that cause permanent damage, because it may prove to be an important factor in our interventions.
References
Alway, Y., McKay, A., Ponsford, J., & Schönberger, M. (2012), Expressed emotion and its relationship to anxiety and depression after traumatic brain injury. Neuropsychological Rehabilitation, 22(3), 374–390. https://doi.org/10.1080/09602011.2011.648757.
Barrowclough, C., & Hooley, J. M. (2003), Attributions and expressed emotion: A Review. Clinical Psychology Review, 23(6), 849–880. https://doi.org/10.1016/s0272-7358(03)00075-8.
Bressi, C., Porcellana, M., Pedrinazzi, C., Manoussakis, C., Marinaccio, P., Magri, L., & Inama, G. (2009), Expressed emotion in wives of myocardial infarction patients: An exploratory feasibility study. Journal of Cardiovascular Medicine, 10(10), 752–757. https://doi.org/10.2459/jcm.0b013e32832cae71.
Brown, George W. (1959). Experiences of discharged chronic schizophrenic patients in various types of Living Group, The Milbank Memorial Fund Quarterly, 37(2), 105. https://doi.org/10.2307/3348588.
Brown, G. W., Monck, E. M., Carstairs, G. M., & Wing, J. K. (1962), Influence of family life on the course of schizophrenic illness. Journal of Epidemiology & amp; Community Health, 16(2), 55–68. https://doi.org/10.1136/jech.16.2.55.
Butzlaff, R. L., & Hooley, J. M. (1998), Expressed emotion and psychiatric relapse. Archives of General Psychiatry, 55(6), 547. https://doi.org/10.1001/archpsyc.55.6.547.
Fichter, M. M., Glynn, S. M., Weyerer, S., Liberman, R. P., & Frick, U. (1997), Family climate and expressed emotion in the course of alcoholism. Family Process, 36(2), 203–221. https://doi.org/10.1111/j.1545-5300.1997.00203.x.
Fogler, J. M., Tompson, M. C., Steketee, G., & Hofmann, S. G. (2007), Influence of expressed emotion and perceived criticism on cognitive-behavioral therapy for social phobia. Behavior Research and Therapy, 45(2), 235–249. https://doi.org/10.1016/j.brat.2006.03.002.
Glynn, S. M., Randolph, E. T., Eth, S., Paz, G. G., Leong, G. B., Shaner, A. L., & Strachan, A. (1990), Patient psychopathology and expressed emotion in Schizophrenia. British Journal of Psychiatry, 157(6), 877–880. https://doi.org/10.1192/bjp.157.6.877.
Gottschalk, L. A., & Gleser, G. C. (1969), The Measurement of Psychological States through the Content Analysis of Verbal Behavior. https://doi.org/10.1525/9780520376762.
Marks, M., Wieck, A., Checkley, S., & Kumar, C. (1996), How does marriage protect women with histories of affective disorder from post-partum relapse? British Journal of Medical Psychology, 69(4), 329–342. https://doi.org/10.1111/j.2044-8341.1996.tb01876.x.
Stirling, J., Tantam, D., Thomas, P., Newby, D., Montague, L., Ring, N., & Rowe, S. (1991), Expressed emotion and early onset schizophrenia: A one year follow-up. Psychological Medicine, 21(3), 675–685. https://doi.org/10.1017/s0033291700022315.
Tομαράς Β., Μαυρέας Β. (1990), Σχιζοφρένεια και οικογένεια. Ο ρόλος της οικογένειας στην πορεία και τη θεραπεία της σχιζοφρένειας. Ιατρική, 57 (3), 238-246.
Wamboldt, M. Z., & Wamboldt, F. S. (2000), Role of the family in the onset and outcome of Childhood Disorders: Selected Research Findings. Journal of the American Academy of Child & Adolescent Psychiatry, 39(10), 1212–1219. https://doi.org/10.1097/00004583-200010000-00006.
Wearden, A. J., Tarrier, N., Barrowclough, C., Zastowny, T. R., & Rahill, A. A. (2000), A review of expressed emotion research in health care. Clinical Psychology Review, 20(5), 633–666. https://doi.org/10.1016/s0272-7358(99)00008-2.
Weddell, R. A. (2010). Relatives’ criticism influences adjustment and outcome after traumatic brain injury, Archives of Physical Medicine and Rehabilitation, 91(6), 897–904. https://doi.org/10.1016/j.apmr.2010.01.020.
Zabala, M. J., Macdonald, P., & Treasure, J. (2009), Appraisal of care giving burden, expressed emotion and psychological distress in families of people with eating disorders: A systematic review. European Eating Disorders Review, 17(5), 338–349. https://doi.org/10.1002/erv.925.
Zigmond, A. S., & Snaith, R. P. (1983), The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Table 1. Critical Attitude at 5MSS