Bergamo (Italy), October 31 - November 5, 2022

Participants from five different European countries (Belgium, France, Greece, Italy, and Spain) shared their experiences, communicating in different languages and understanding each other with the feeling of belonging to a unique culture and an ancient tradition of valuing and respecting cultural differences. Participants experienced the richness and complexity of being diverse and inclusive in the same time, finding common values and sharing questions, needs, and innovative practices which can be reproduced in other countries. A strong will of exchanging experiences and learning from each other emerged during the week.
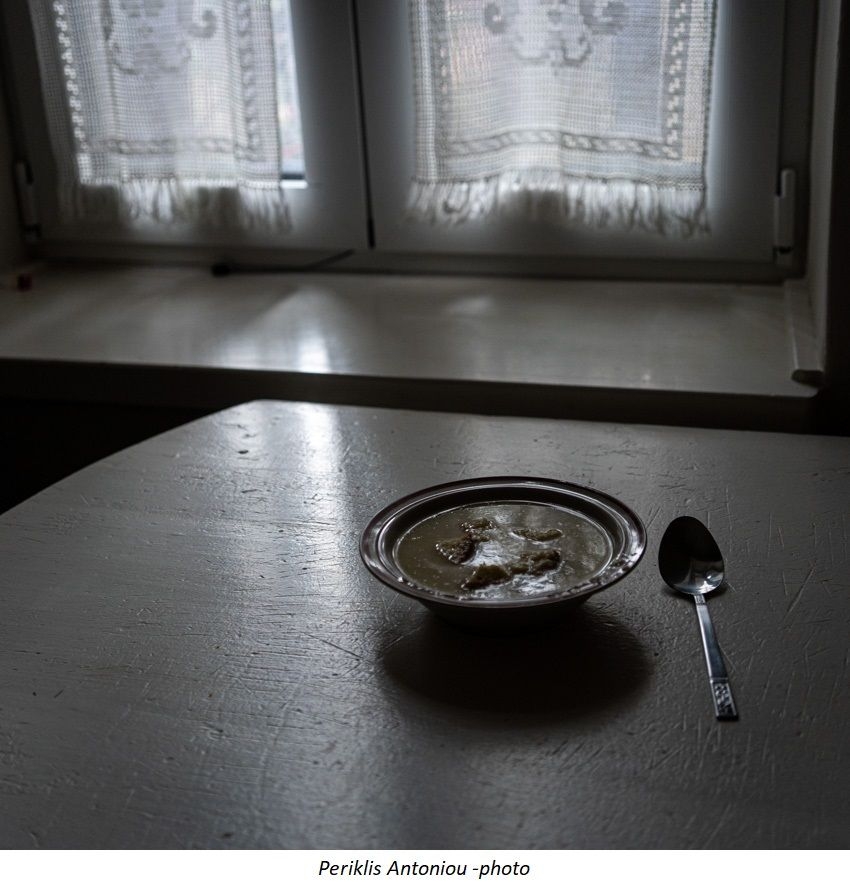
When we speak of "mental health" we are not speaking only of mental disorders such as addiction or other psychiatric conditions, or of psychiatric institutions and services: we are speaking of the life in our communities, of young adults that everyday deal with a difficult world, particularly after the years of isolation due to the COVID-19 pandemic. However, in our week of the YAMI project in Bergamo we focused also on more difficult situations, such as those we deal with in our Mental Health Services.
YAMI participants agreed on the following statements regarding the improvement of youth mental health throughout Europe:
-
Promotion of well-being and improvement of quality of life, with particular focus on the social, economic, cultural, educational and health aspects related to the life of young adults. Creation of contexts for equal opportunities that are pluralistic and inclusive, and that encourage active citizenship, fight social stigma and discrimination regarding religion, ethnicity, gender, social class, etc. Spaces for autonomous self-organization of young adults should be promoted and sustained also with public funding.
-
Prevention of psychological problems should be emphasized. Preventive actions should aim to improve mental health literacy, in order to facilitate early intervention in youth population, i.e., early detection, facilitating young people help seeking for themselves and/or families and friends. Community and local stakeholders should provide spaces for young people and plan prevention activities. Prevention implies an investigation on screening methods in order to identify risk factors such as drug and alcohol abuse, and on modalities of reaching out. Sensibilization campaigns on psychological problems with the use of social media (particularly those used by young generations) could be very useful to young adults, especially regarding abuse, neglect, discrimination, family disruption, bullying, violence, negative influence of some types of commercial advertising, etc. Focus should be on resources and resilient factors at individual, family and community level (and not on the problem during the prevention phase). Collaboration with schools, local, cultural, and sports associations is needed, combating social isolation and promoting civic awareness, green culture, education for peace and democracy, independent and critical thinking.
-
Early intervention should be targeted not only on early psychoses, but also on clinical or subclinical (sub-threshold) common mental health difficulties such as anxiety and mood disturbances. The presence of mental health professionals (psychologists and counselors) at school, colleges and universities is of paramount importance. It seems essential to develop outpatient services to avoid hospitalizations as much as possible and to propose solutions adapted to the situation related to the context of young adults.
-
Specific "youth centers" or "open houses" for the treatment of various psychopathologies should be implemented in the community. Examples are the Balance Homes in Israel where patients can regain their emotional balance after a psychological crisis, or the Soteria Houses founded in the early 1970s in California by Loren Mosher, later implemented in various countries; these houses provide space for people experiencing psychological distress or crisis and are based on a "recovery" model, with primarily non- medical staff engaging residents’ social networks and finding meaning in the subjective experience of distress, with minimal use of medication and no restraint. Attention to the patients’ social environment should focus also on trans-cultural aspects. In these centers, that could be accessed also without a medical referral, guests should find peers and perform various recreational and cultural activities they like the most (such as art, sport, meditation, body works, reading, writing, poetry, etc.). Also, the architecture of these houses should be attractive to young adults. Former guests could play a role as members of the staff in adding their help to peers during the therapeutic process.
-
A wide range of therapeutic opportunities should be offered. Beside youth centers and open houses, there should be various therapeutic modalities such as hospitals, therapeutic communities, day-centers, out-patient clinics, outreaching teams with home visits, etc., in order to assist young adults with psychotic episodes and other psychological sufferings. Non-residential care should be emphasized; residential treatment, if needed, should be short, medium, and long-term, possibly in the same area where the patient lives and with an involvement of his/her social network; ideally, inpatient treatment should be provided in units specifically designed for young adults, in order to avoid age differences among patients hospitalized in the same ward. Mobile teams can be particularly suited to support – in the community and at home, for a short period (about a month) – young adults going through a crisis who have difficulties in obtaining psychiatric help; these teams can create a bridge between the health and social areas, with the aim of reducing stigma in contexts of great flexibility. Post-hospitalization programs should aim to improve recovery through specific actions like more suitable school programs, coaching for students, vocational guidance, supported jobs, job placement, etc. The role of teamwork should be valued, and teams should move from a multidisciplinary to an interdisciplinary functioning, and different professionals (psychiatrists, psychotherapists, psychologists, counselors, social workers, psychiatric rehabilitation specialists, professional educators, nurses, art therapists, body workers, etc.) could be utilized in the process of care at various levels, according to their expertise, in order also to allow young people to choose which kind of care they need and desire.
-
Treatment should be based on different modalities, verbal and non-verbal; medication, when needed, should always be combined with a psychological understanding of the patient’s symptoms within his/her life’s history. The role of behavioral activation is important. As Franco Basaglia (the leader of the Italian movement for psychiatric reform) used to say, what patients need is not only to talk about something, but to do things, to be personally and emotionally involved in some activities; in fact, as research has shown, emotions, rather than cognitions, have the major role in promoting change. The therapeutic relationship should foster an ongoing co-construction of life narratives and meanings within supportive interdisciplinary teams with a particular attention to the sense of belonging and basic needs of young adults. Treatment should be focused on the patient’s resilience and strengths, supporting empowerment, social recovery and social reintegration, and not on traditional psychiatric diagnosis; to this regard, diagnoses which increase social stigma should be avoided, and a transdiagnostic approach should be preferred (for example, attention to issues of affect regulation and attachment), considering also that many DSM diagnoses have some reliability but lack validity. Families should be considered partners: family support, family therapy and multifamily groups should be part of the routine work. Group therapy is often underutilized in mental health services, and should be implemented as most as possible because it is very useful and also cost-effective. Since in the public sector the practice of individual long-term psychotherapy is problematic because of the unavailability of an adequate number of psychological therapists, a service of short-term individual psychotherapy should be activated in every Mental Health Center. A service of brief psychotherapy would allow a larger number of users to have an experience of better understanding their inner world and the causes of their suffering, also with the aim of preventing future emotional difficulties. Research has shown that brief psychotherapies conducted by well trained therapists are effective in common mental disorders such as anxiety and depression, and frequently more effective than medication. National and international online group seminars for young adults with similar psychological problems should be arranged in order to exchange experiences. Also self-help groups are very important; in fact, research shows that self-help groups are extremely effective for specific psychological problems, and at times are more efficacious than professional treatments. An important method of intervention in early psychosis is the Open Dialogue approach developed by Seikkula’s team in Western Lapland (Finland), now experimented also in other countries; this method is based on meetings within 24 hours after contact that includes as many significant people as possible from the patient’s family and social network, with the aim of generating dialogue and putting words to the experiences embodied in the patient’s psychotic symptoms.
-
There is no treatment without "love". We are well aware that the term "love" has various meanings in different countries and cultures, and that this statement may seem simplistic or naïve, but it is at the heart of many theories of psychotherapeutic technique developed in the course of the twentieth century: what we mean is that in the approach to psychological suffering an important aspect, maybe the most important one, is the role of affectivity, i.e., the creation of a positive emotional bond, the feeling on the part of the patient that the staff member sees him/her as a valuable person despite the negative affects and great difficulties that at times are present. When we talk of "love" we mean that, in order to be efficacious, staff members should always try to maintain, also with a difficult patient, an ongoing relationship characterized by stability, consistency, warmth, acceptance, complicity, humor, joy, and play. There is no change without positive feelings. Of course, it is not easy to work with a difficult patient, but an important aspect of therapy consists precisely in the understanding, on the part of the therapist, of his/her negative feelings and in cultivating the ability to reflect and work on his/her emotional reactions.
-
Mental health professionals should themselves receive "care": they should receive adequate salaries and, most importantly, appropriate training in the most effective therapeutic techniques, continuous education and group supervision (as well as "inter-vision", i.e., peer groups of professionals that meet regularly to discuss difficult cases and emotional problems they might have in the relationship with difficult patients). Also individual supervision should be provided in case of need. Conferences, courses, meetings and international exchanges are extremely useful in order to grow and avoid cultural isolation, demotivation, and burn-out.
-
Services and treatment facilities should continue to receive appropriate funding, in order to guarantee continuity and variety of care.
-
Last, but not least, empirical research is extremely important. Guided by expert researchers, each team should carry out research projects with the aim of validating specific interventions or approaches for the prevention and treatment of psychological problems of young adults.
References
Allen, J. G. (2001). Traumatic relationships and serious mental disorders. John Wiley & Sons Ltd.
Allen, J. G. (2008). Coping with trauma: Hope through understanding. American Psychiatric Pub.
Allen, J. G. (2018). Mentalizing in the development and treatment of attachment trauma. Routledge. American Psychological Association (2013). Recognition of psychotherapy effectiveness. Psychotherapy, 50, 1: 102-109 (www.apa.org/about/policy/resolution-psychotherapy) (trad. it.: Riconoscimento dell’efficacia della psicoterapia. Psicoterapia e Scienze Umane, 2013, 47, 3: 407-422. [www.francoangeli.it/riviste/Scheda_Rivista.aspx?IDArticolo=49182&Tipo=Articolo%20P DF&lingua=it&idRivista=34]).
Anderson, H. (1997). Conversation, language, and possibilities: A postmodern approach to therapy. Basic Books.
Andolfi, M. (1991). Terapia familiar: un enfoque interaccional. Paidós. Åsbø, G, Ueland, T., Haatveit, B., Bjella, T., Flaaten, C.B., Wold, K.F., Widing, L., Engen, M.J., Lyngstad, S.H., Gardsjord, E., Romm, K.L., Melle, I., Simonsen, C. (2022). The Time is Ripe for a Consensus Definition of Clinical Recovery in First-episode Psychosis: Suggestions Based on a 10-Year Follow-up Study. Schizophr Bull. 48(4), 839-849. doi: 10.1093/schbul/sbac035.
Asen, E., & Schuff, H. (2006). Psychosis and multiple family group therapy. Journal of Family Therapy, 28(1), 58–72. https://doi.org/10.1111/j.1467-6427.2006.00337.x
Badaracco, J. E. G. (2000). Psicoanálisis multifamiliar: los otros en nosotros y el descubrimiento del sí mismo. Paidós.
Badenoch, B., & Gantt, S. P. (Eds.). (2018). The interpersonal neurobiology of group psychotherapy and group process. Routledge.
Barbato A., Biondi M., Corbo M., de Girolamo G., Favaretto G., Garattini S., Migone P., Moderato P., Monzani E., Veltro F. & Sanavio E. (2022). Editorial: The Italian Consensus Conference on psychological therapies for anxiety and depressive disorders: Findings and recommendations. Epidemiology and Psychiatric Services, 31, in press.
Borcsa, M. & Pomini, V. (2020). La diffusione delle pratiche digitali nella psicoterapia sistemica: Lo stato dell'arte in Europa e oltre. In Manfrida, G. Albertini, V. & Eisenberg, E. (eds.) La clinica e il web. Risorse tecnologiche e comunicazione psicoterapeutica online. Franco Angeli. pp. 37-60.
Bowen, M. (1991). De la familia al individuo: la diferenciación del sí mismo en el sistema familiar. Paidós.
Breda, C. S., & Riemer, M. (2012). Motivation for Youth’s Treatment Scale (MYTS): A new tool for measuring motivation among youths and their caregivers. Administration and Policy in Mental Health and Mental Health Services Research, 39(1), 118-132.
Burbach, F. (2018). Family therapy and schizophrenia: A brief theoretical overview and a framework for clinical practice. BJPsych Advances, 24(4), 225-234. doi:10.1192/bja.2017.32.
Burbach, F., & Stanbridge, R. (2006). Somerset’s family interventions in psychosis service: an update. Journal of Family Therapy, 28(1), 39–57. doi:10.1111/j.1467-6427.2006.00336.x
Campaioli, G., Sala, E., Simonelli, A., & Pomini V. (2017). The dual value of the web: Risks and benefits of the use of the internet in disorders with a self-destructive component. Contemporary Family Therapy, 39 (4), 301-313.
Canevaro, A., & Bonifazi, S. (2011). Il gruppo multifamiliare: un approccio esperienziale (Ser. Famiglie: psicoterapia e dintorni). Armando Ed. Tondi, F. Recensione-saggio di: Jaakko Seikkula, Il dialogo aperto. L'approccio finlandesealle gravi crisi psichiatriche. Cura e trad. di Chiara Tarantino. Roma: Fioriti, 2014. Psicoterapia e Scienze Umane, 49(3), 493–499. DOI: 10.3280/PU2015-003012 (www.francoangeli.it/riviste/SchedaRivista.aspx?IDArticolo=54798&idRivista=34)
Cozolino, L. (2015). Why Therapy Works: Using Our Minds to Change Our Brains (Norton Series on Interpersonal Neurobiology). WW Norton & Company.
Csillag, C., Nordentoft, M., Mizuno, M., McDaid, D., Arango, C., Smith, J. & Jones, P. B. (2018). Early intervention in psychosis: From clinical intervention to health system implementation. Early Intervention in Psychiatry, 12(4), 757-764. doi: 10.1111/eip.12514
Davoine, F. (1992). La Folie Wittgenstein. Paris: École lacanienne de psychanalyse [E.P.E.L.]
DeLuca, J.S., Yang, L.H., Lucksted, A.A., Yanos, P., & DeVylder, J. (2021). Reducing Stigma Among Youth at Risk for Psychosis: A Call to Action. Schizophrenia Bulletin, 47(6), 1512–1514.
Edelstein, C. (2013). L’epistemologia del “Noi” nel modello sistemico pluralista: il riconoscimento dell’Altro come processo circolare, dinamico e riflessivo nei percorsi di aiuto. Riflessioni sistemiche, (8), http://www.aiems.eu/files/edelstein_8.pdf
Edelstein, C. (2013). L’esperienza di Shinui e il modello sistemico pluralista in ambito interculturale. m@gm@ - Rivista Internazionale di Scienze Umane e Sociali, 11(3). http://www.analisiqualitativa.com/magma/1103/index.htm Edelstein, C. (2017). Un movimento umanistico emergente: il Coordinamento Italiano dei Professionisti della Relazione di Aiuto (CIPRA). m@ gm@-Rivista Internazionale di Scienze Umane e Sociali, 15(2). http://www.analisiqualitativa.com/magma/1702/1702.pdf
Edelstein, C. (2017). Movimento Umanistico e Relazione d’Aiuto: verso una sensibilità collettiva. m@gm@- Rivista Internazionale di Scienze Umane e Sociali, 15(2) http://www.analisiqualitativa.com/magma/1502/index.htm Edelstein, C. editor (2018). Le diverse professioni nella relazione di aiuto. Un movimento emergente. Aracne. Edelstein, C. (2019). Rispecchiamenti e sguardi altrove: la legge 180 attorno al mondo.m@gm@-Rivista Internazionale di Scienze Umane e Sociali, 17(2). http://www.analisiqualitativa.com/magma/1702/articolo_01.htm
Edelstein, C. (2019). Istituzionalizzazione / deistituzionalizzazione: sguardi reciproci sulla legge 180 in Europa e nel mondo. m@gm@ - Rivista Internazionale di Scienze Umane e Sociali, 17(2), http://www.analisiqualitativa.com/magma/1702/1702.pdf
Fusar-Poli, P., Salazar de Pablo, G., Correll, C. U., Meyer-Lindenberg, A., Millan, M. J., Borgwardt, S., Arango, C. (2020). Prevention of Psychosis. JAMA Psychiatry, 77(7), 755. doi:10.1001/jamapsychiatry.2019.4779
Galanis, D., Selakovic, M., Feretzaki, A., & Pomini, V. (2020). Multiple family group therapy in an early intervention setting for psychosis: A pilot group in a public hospital. Systemic Thinking & Psychotherapy, 17, 55-71.
Garcia del Castillo, I., López García, S., Pérez-Balaguer, A., Gojman-de-Millán, S., Herreman, C., & Sroufe, L. A. (2018). La teoría del apego: investigación e intervención en distintos contextos socioculturales. Fondo de cultura económica.
González Pardo, H., & Pérez Álvarez, M. (2007). La invención de los trastornos mentales. Escuchando al fármaco o al paciente. Alianza. Gruppo di lavoro “Consensus sulle terapie psicologiche per ansia e depressione” (2022). Consensus Conference sulle terapie psicologiche per ansia e depressione. Documento finale (Consensus Conference on psychological therapies for anxiety and depression. Final document). Roma: Istituto Superiore di Sanità. www.iss.it/documents/20126/0/Consensus_1_2022_IT.pdf (English Edition: www.iss.it/documents/20126/0/Consensus_1_2022_EN.pdf).
Guy, J. D. (1995). La vida personal del psicoterapeuta: el impacto de la práctica clínica en las emociones y vivencias del terapeuta (Vol.126). Grupo Planeta (GBS).
Jurewicz, I. (2015). Mental health in young adults and adolescents – supporting general physicians to provide holistic care. Clinical Medicine, 15(2), 151–154. https://doi.org/10.7861/clinmedicine.15-2-151 Kirsch I. (2009). The Emperor’s New Drugs: Exploding the Antidepressant Myth. London: The Bodley Head (trad. it.: I farmaci antidepressivi: il crollo di un mito. Dalle pillole della felicità alla cura integrata. Tecniche Nuove, 2012).
Kollias, K., Xenaki, L., Vlachos, I., Dimitrakopoulos, S., Kosteletos, I., Nianiakas, N., Stefanatou, P., & Stefanis, N.C. (2020). The development of the Early Intervention in Psychosis (EIP) outpatient unit of Eginition University Hospital into an EIP Network. Psychiatriki, 31,177–182.
Kosyluk, K. A., Al-Khouja, M., Bink, A., Buchholz, B., Ellefson, S., Fokuo, K. & Corrigan, P. W. (2016). Challenging the stigma of mental illness among college students. Journal of Adolescent Health, 59(3), 325-331.
Laqueur, H. P., Wells, C. F., & Agresti, M. (1969). Multiple-Family Therapy in a State Hospital. Psychiatric Services, 20(1), 13–20. doi:10.1176/ps.20.1.13
Layard R. & Clark D.M. (2014). Thrive: How Better Mental Health Care Transforms Lives and Saves Money. Foreword by Daniel Kahneman. Princeton, NJ: Princeton University Press (Italian translation: Il potere della terapia psicologica. Come migliorare la vita delle persone e della società. Giunti, 2022).
Lemmens, G. M. D., Eisler, I., Migerode, L., Heireman, M., & Demyttenaere, K. (2007) Family discussion group therapy for major depression: a brief systemic multi-family group intervention for hospitalized patients and their family members. Journal of Family Therapy, 29, 49–68.
Linares, J. L., & Vallarino, D. (2008). Schizophrenia and eco-resilience. Journal of Systemic Therapies, 27(3), 16–29.
Lobo, A. O. (2016). Hacia una Psiquiatría Crítica: excesos y alternativas en salud mental. Editorial Grupo 5.
Loh, C., Liang, W., Lee, H., & Tang, C. (2021). Development of Multi‐Family Therapy for First Episode Psychosis in Singapore. Journal of Family Therapy. doi:10.1111/1467- 6427.12329
Lykomitrou, A., Souliotis, K., Saridi, M., & Stylianidis, S. (2019). The mobile mental health units services utilization in the northeastern and western cyclades, Greece. International Journal of Caring Sciences, 12(1), 40–48.
Migone P. (2005). Farmaci antidepressivi nella pratica psichiatrica: efficacia reale. Psicoterapia e Scienze Umane, 39, 3: 312-322.Gedisa (www.francoangeli.it/riviste/SchedaRivista.aspx?IDArticolo=25358&idRivista=34). Una versione del 2009 su Internet: www.psychomedia.it/pm/modther/probpsiter/ruoloter/rt112- 09.htm. Migone P. (2017). The influence of pharmaceutical companies. Research in Psychotherapy: Psychopathology, Process and Outcome (RIPPPO), 20, 2: 136-138. Open-access: http://researchinpsychotherapy.org/index.php/rpsy/article/view/276/222.
Minuchin, S. (1974). Familias y terapia familiar. Gedisa.
Mount, J., Lister, A., & Bennun, I. (2004). Identifying the mental health needs of looked after young people. Clinical Child Psychology and Psychiatry, 9(3), 363-382.
Norcross J.C., editor (2011). Psychotherapy Relationships That Work: Evidence-Based Responsiveness. Second Edition. New York: Oxford University Press (First Edition: Psychotherapy Relationships That Work: Therapist Contributions and Responsiveness to Patients. New York: Oxford University Press, 2002) (trad. it. della seconda edizione [2011]: Quando la relazione psicoterapeutica funziona... Vol. 1: Ricerche scientifiche a prova di evidenza. Vol. 2: Efficacia ed efficienza dei trattamenti personalizzati. Roma: Sovera, 2012).
Norcross, J. C., & Lambert, M. J. (2011). Psychotherapy relationships that work II. Psychotherapy, 48(1), 4–8.
Pantelidou, S., Stylianidis, S., & Manolesou, S. (2019). Family functioning and depression among Albanian migrants and Greeks in a rural area in Greece. Dialogues in Clinical Neuroscience & Mental Health, 2(4), 206-219.
Pantelidou, S.; Manolesou, S.; Apostolopoulou, A.; Giannakopoulou, K.; Stylianidis, S. (2021). Albanian Migrants in Cyclades: Contact with Mental Health Services and Implications for Practice. Psych, 3, 916–930. https://doi.org/10.3390/psych3040057
Peritogiannis, V., Fragouli-Sakellaropoulou, A., Stavrogiannopoulos, M., Filla, I., Garmpi, A., Pantelidou, S., Samakouri, M. (2022). Coordinating Committee of the Mobile Mental Health Units, The role of the Mobile Mental Health Units in mental healthcare delivery in rural areas in Greece: current challenges and prospects, Psychiatriki doi:https://doi.org/10.22365/jpsych.2022.084
Pomini V., Akalestou M.I., Tomaras V., Charalabaki K. (2016). Systemic training for ‘frontier’ mental health professionals: An experience from Greece, in the face of the financial crisis. Human Systems, 27 (1), 21-37.
Pomini, V. (2020). Families and Therapists in the vortex of the Corona Virus Pandemic. Systemic Thinking & Psychotherapy, 16, 1-16 https://hestafta.org/journal/systemic-thinkingpsychotherapy/issue-16/?lang=en
Riemer, M., Athay, M. M., Bickman, L., Breda, C., Kelley, S. D. & Vides de Andrade, A. R. (2012). The Peabody Treatment Progress Battery: History and methods for developing a comprehensive measurement battery for youth mental health. Administration and Policy in Mental Health and Mental Health Services Research, 39(1), 3-12.
Sanavio, E. (2022). Una Consensus Conference sulle terapie psicologiche per ansia e depressione (A Consensus Conference on psychological therapies for anxiety and depressive disorders). Psicoterapia e Scienze Umane, 56, 1: 11-20. (www.francoangeli.it/riviste/SchedaRivista.aspx?IDArticolo=70603&Tipo=Articolo%20PD F&lingua=it&idRivista=34). Seikkula, J. (2019). Psychosis Is Not Illness but a Survival Strategy in Severe Stress: A Proposal for an Addition to a Phenomenological Point of View. Psychopathology, 1–8. doi:10.1159/000500162
Seikkula, J. & Olson, M. E. (2003). The open dialogue approach to acute psychosis: its poetics and micropolitics. Family Process, 42(3), 403–418. https://doi.org/10.1111/j.1545-5300.2003.00403.x
Selakovic, M., Galanis, D., Frankiadaki, E., Theodoropoulou, P., & Pomini, V. (2020). Athens Multifamily Therapy Project. Schizophrenia Bulletin, 46 (Suppl 1): S303. doi: 10.1093/schbul/sbaa029.747.
Sempere, J. & Fuenzalida, C. (2017). Interfamily Therapy. From Family Therapy to Therapy among others. In Employment, Training and Research in Psychiatry and Mental Health: An innovative Tutoring Project in Europe, pp 127-143. L’Harmattan, Logiques Sociales.
Sempere, J., & Fuenzalida, C. (2017). Terapias multifamiliares: El modelo interfamiliar: la terapia hecha entre todos. Psimática.
Shedler, J. (2010). The efficacy of psychodynamic therapy. American Psychologist, 65, 2: 98-109. Open-access: www.apa.org/pubs/journals/releases/amp-65-2-98.pdf
Solomon, M. F. & Siegel, D. J. (2017). How People Change: Relationships and Neuroplasticity in Psychotherapy. WW Norton & Company.
Torres, B., Causadias, J. M. & Posada, G. (Eds.). (2014). La teoría del apego: investigación y aplicaciones clínicas. Psimática.
Valentine, L., McEnery, C., O’Sullivan, S., D’Alfonso, S., Gleeson, J., Bendall, S. & Alvarez‐Jimenez, M. (2021). Young people’s experience of online therapy for first‐episode psychosis: A qualitative study. Psychology and Psychotherapy: Theory, Research and Practice. doi:10.1111/papt.12356
Vetere, A. & Dallos, R. (2012). Apego y terapia narrativa: un modelo integrador. Ediciones Morata.
Wallin, D. J. (2012). El apego en psicoterapia. Desclée de Brouwer.
Webber, M, & Fendt-Newlin M. (2017). A review of social participation interventions for people with mental health problems. Social Psychiatry and Psychiatric Epidemiology. 52(4), 369-380. doi: 10.1007/s00127-017-1372-2.
Whitaker, R. (2010). Mad in America. Bad science, bad medicine, and the enduring mistreatment of the mentally ill. Basic Books.
Xenaki, L.-A., Kollias, C. T., Stefanatou, P., Ralli, I., Soldatos, R.-F., Dimitrakopoulos, S., Stefanis, N. C. (2020). Organization framework and preliminary findings from the Athens First-Episode Psychosis Research Study. Early Intervention in Psychiatry, 14(3):343-355. doi:10.1111/eip.12865.
Yalom, I. D. (2010). Psicoterapia existencial y terapia de grupo. Paidós.
Yalom, I. D., & Vinogrador, S. (1996). Guía breve de psicoterapia de grupo. Paidós.
Zerbetto, R. (2020). ENTRY: progetto Europeo sulla Prevenzione della Violenza tra i Giovani. Monografie di Gestalt, 8.